How Patients and Clinicians Really Feel About Telehealth One Year Later

Telehealth has tremendous potential to improve patient care, but we still have much to learn. The pandemic forced us into a massive experiment. So, what have we learned about telehealth over the past crazy, challenging, disorienting, disruptive year?
MHQP has dedicated itself to this help answer this question. First, we launched “Together for Better Telehealth,” a series of surveys designed to help clinicians share what they were learning from their telehealth experiences and to help the whole profession rapidly adapt to this new way of providing care. Then in June 2021, we fielded our “Telehealth One Year Later” follow-up surveys to evaluate telehealth experiences for both clinicians and patients. 238 clinicians and 125 patients responded.
When added to MHQP’s long history and expertise with measuring and evaluating patient experiences, these initiatives put MHQP in a unique position to provide a summative report on the pandemic telehealth experiment. The rich insights and improvement ideas we collected in these surveys give a better sense of how both clinicians and patients are experiencing telehealth and offer important reflections on what we still need to do to ensure telehealth lives up to its full potential.
Many of our topline observations may seem obvious to anyone who has been involved with telehealth over the past year-and-a-half. Yet, we believe it is important to provide a comprehensive synthesis of the results so that all may learn from them.
Key Findings – Overall Satisfaction
1. Patients liked the telehealth experience much more than clinicians did.
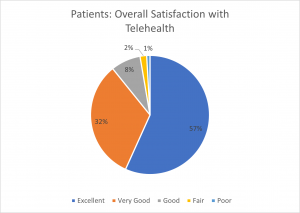
The patients we surveyed had an overwhelmingly positive experience with telehealth. When asked about their overall satisfaction with telehealth, 89% of patients who responded said it was either “Excellent” or “Very Good.” Only 3% said it was either “Fair” or “Poor.”
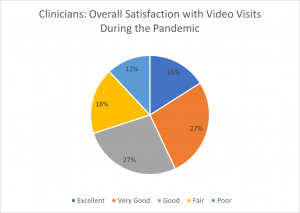
We asked providers about their experiences with video and telephone separately. In contrast to patients, only 43% of providers reported that their experience with video was either “Excellent” or “Very Good,” and 46% of providers gave their phone experience one of those ratings. 30% and 27% of providers gave their video and phone experiences (respectfully) a rating of “Fair” or “Poor.”
2. Patients had a stronger belief that telehealth is important to their future care than did clinicians.
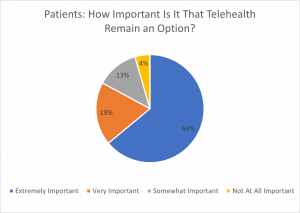
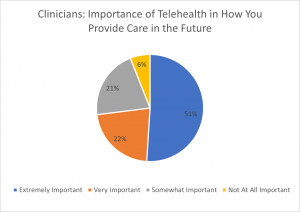
Along the same lines, 83% of patients believe it is “Extremely Important” or “Very Important” that telehealth remains an option in the future. In contrast, only 73% of clinicians believe telehealth will be “Extremely Important” or “Very Important” to how they provide patient care in the future.
Key Findings – Patients
1. Most patients loved telehealth for one reason: convenience
Without a doubt, convenience is the principal reason patients liked telehealth. Patients appreciated being able to connect with their clinicians remotely for most care because it allowed them to avoid the hassle of getting to their provider’s office. When asked what they found most satisfying about using video and/or telephone for their healthcare visit, 88% said something related to convenience – e.g., improved access, time savings, increased flexibility, etc.
Click HERE to see some of the verbatim comments that illustrate this point.
2. Patients understood that telehealth is not practical in all clinical circumstances.
While patients appreciate the convenience of telehealth, they also recognize virtual care is not optimal for situations that require a “hands-on” encounter with the provider. Patients felt that telehealth worked especially well for behavioral health visits and follow-up visits that don’t require a physical exam. They recognize that the telehealth medium is not ideal for many encounters (e.g., annual physical, dermatology, ophthalmology), but hope to strike an effective balance between in-person and telehealth care in the future.
Click HERE for sample comments.
3. Some patients appreciated telehealth for quality and safety reasons.
Beyond the convenience factor that telehealth offered patients, some patients pointed out that it also gave them an added sense of security knowing they could remain socially distanced during the pandemic while not sacrificing clinical quality. Some patients seemed to feel that telehealth actually improved the quality of care in some circumstances where ease of access was essential. For example, one patient stated that it allowed for better management of their blood pressure issues; and another indicated that it was sometimes easier to talk to their child’s pediatrician via telehealth when their child is sick.
Click HERE for sample comments.
4. Technology issues hindered some encounters.
Despite the predominance of positive experiences, many patients commented that the technology left much to be desired. Without question, the technology offered by some practices was a significant challenge for patients and some patients felt their provider was ill-prepared for managing the technology. In addition, lack of reliable broadband service and “choppy reception” made it difficult for some patients to fully engage with providers in this way.
Click HERE for sample comments.
Key Findings – Providers
1. Provider satisfaction with telehealth varied considerably based on the provider’s network affiliation.
We compared results for six networks, each of which had more than 10 providers respond to the survey. It is important to note that this was a convenience sample of Massachusetts clinicians and the counts in each network were small, so findings should be interpreted with a degree of caution. However, these results seem to indicate that the organizational approach and choice of telehealth technology may have a significant impact on provider experience and suggest that they are important opportunities for improvement in network-specific telehealth performance.
The percent of clinicians who said their experience connecting with patients by either video or telephone was “Excellent” or “Very Good” ranged from as low as 15% for one network to as high as 73% for another:
| % Excellent + Very Good | ||
|---|---|---|
| Video | Telephone | |
| Statewide Average | 43% | 46% |
| Network A | 36% | 27% |
| Network B | 67% | 52% |
| Network C | 15% | 54% |
| Network D | 73% | 36% |
| Network E | 42% | 25% |
| Network F | 67% | 44% |
It is also interesting to note the differences between video and telephone experiences in some networks. For Network C, only 15% of clinicians reported having “Excellent” or “Very Good” experiences with video, while 54% said they had “Excellent” or “Very Good” experiences on telephone. For Network D, essentially the opposite was true: only 73% of clinicians reported having “Excellent” or “Very Good” experiences with video, while only 36% said they had “Excellent” or “Very Good” experiences on telephone.
We also found important differences in the extent to which clinicians in the network view telehealth to be important to how they provide care in the future. The percentages saying it was “Extremely Important” or “Very Important” ranges from a low of 54% to a high of 91%:
| % Extremely Important + Very Important | |
|---|---|
| Statewide Average | 73% |
| Network A | 80% |
| Network B | 91% |
| Network C | 70% |
| Network D | 75% |
| Network E | 54% |
| Network F | 84% |
2. Clinicians bemoaned telehealth technology more than patients did.
The technological challenges associated with telehealth seemed to completely overshadow the positive aspects of the care experience for many clinicians. When we asked clinicians what they found most challenging about using video and/or telephone for conducting patient visits, 53% responded with something having to do with technology hassles. One even went so far as to say it was a “total disaster” and a “waste of my time and my patient’s time.” Another stated that technical issues “caused me chest pain and caused me to retire sooner than expected.”
Click HERE for sample comments.
3. Some clinicians simply preferred in-person visits.
Many clinicians bemoaned the “reduced closeness/quality of relationship” in telehealth encounters and commented that they missed the human touch associated with in-person visits because it both enables more in-depth clinical evaluation and deeper connection with patients. In one provider’s words, “It’s a very poor substitute for person-to-person interactions.”
Click HERE for sample comments.
4. Yet, many clinicians recognized that telehealth is better in some circumstances.
While many clinicians stated they prefer seeing their patients in person, many also seemed to believe that telehealth is a better medium for certain conditions and certain patients – for example, patients with transportation issues or follow-up care for stable problems. Behavioral health care was also widely seen as effective via telehealth. In general, clinicians seemed to seek an appropriate balance, ensuring the “right” appointments are booked for telehealth while others are booked for in-person visits.
Click HERE for sample comments.
5. And many found unexpected positive aspects of telehealth.
Many clinicians found unexpected benefits and insights from the improved access offered by telehealth. One very interesting finding is that telehealth seemed to reduce no-shows, presumably because of the convenience factor. In addition, some clinicians pointed to the added benefit of seeing the patient while they were comfortable in their own home and familiar surroundings.
Click HERE for sample comments.
