Telehealth Satisfaction: Up for Clinicians, Down for Patients

(October 2022)
Two-and-a-half years since the beginning of the pandemic, what have we learned about telehealth and how can we make it better for everyone? MHQP has endeavored to answer this question throughout the pandemic in multiple ways.
First, we launched “Together for Better Telehealth” in the summer of 2020, a series of surveys to help clinicians share what they were learning from their telehealth experiences.
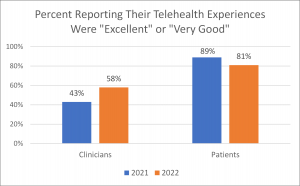
Then, in the summer of 2021, we fielded our “Telehealth One Year Later” surveys to better understand how both patients and clinicians were experiencing telehealth. These surveys exposed a concerning gap between patient satisfaction and clinician satisfaction with regard to telehealth. At that point, 89% of the patients we surveyed reported that their telehealth experience was either “Excellent” or “Very Good.” This stood in stark contrast to the 43% of clinicians who gave their telehealth experiences such high ratings. Patients loved it but clinicians were much less enthusiastic. This enormous satisfaction gap between those serving and those being served was troubling.
This past summer, we fielded another set of surveys for both clinicians (n = 217) and patients (n = 111) to assess how things have changed in the past year. While these surveys involved convenience samples, the data and rich comments we collected offer important reflections on what we still need to do to ensure telehealth lives up to its full potential.
These surveys reveal that clinician satisfaction increased in 2022 versus 2021, while patient satisfaction decreased. Although patients continue to like the telehealth experience in 2022 much more than clinicians do, that gap has narrowed since 2021.
What’s Behind the Increase in Clinician Satisfaction?
58% of clinicians who responded said their overall satisfaction with telehealth visits in the past year was either “Excellent” or “Very Good,” as compared to 43% in 2021. Only 1% of clinicians rated their satisfaction as “Poor” in 2022, as compared to 12% in 2021.
79% of clinicians reported that their personal experiences with telehealth were “Significantly Better” or “Somewhat Better” than at the beginning of the pandemic.
Based on comments from respondents, this improvement seems to be largely driven by two factors:
(Click on the “+” to see comments illustrating each theme)
What’s Behind the Decrease in Patient Satisfaction?
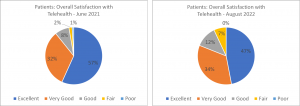
The positive news about clinician satisfaction increasing is tempered by the fact that the percent of patients reporting that their telehealth experience was either “Excellent” or “Very Good” decreased from 89% in 2021 to 81% 2022. 7% of patients rated their satisfaction as “Fair” or “Poor” in 2022, as compared to 3% in 2021. Although patients continue to have high levels of satisfaction with telehealth, the eight point drop in satisfaction in one year is notable.
Based on comments from patients, this decline seems to be driven primary by:
Work To Be Done
Telehealth has tremendous potential to improve access to care for many patients and in many circumstances. Patients continue to have very high levels of satisfaction with telehealth, as we have previously reported, primarily because of the convenience it offers and especially when the clinical situation does not require an in-person visit. Continued focus on technological advancements, policy improvements, and a relentless focus on the patient as the customer will go a long way to restoring and retaining high levels of patient satisfaction with telehealth.
Clinician satisfaction, while improving, still remains relatively low. Great progress appears to have been made over the past few years, and patients and clinicians have become more comfortable with using telehealth, but we still have much work to do to make telehealth a technology that clinicians will consistently turn to and patients can reliably count on for accessing care.
81% of patients and 75% of clinicians responding in 2022 believed that telehealth will be “Extremely Important” or “Very Important” to the future of care.

As we look to that future, we see many opportunities to improve this technology to ensure telehealth lives up to its full potential for both patients and providers.

